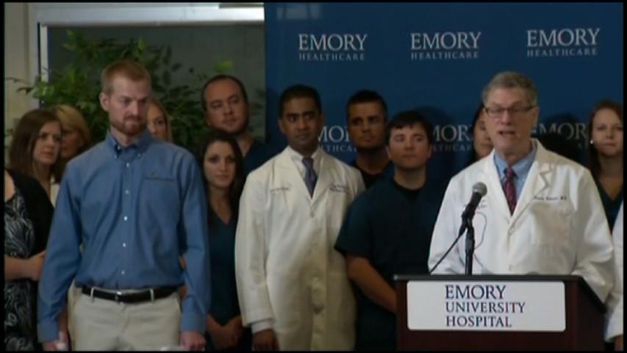
Aug. 21 (Bloomberg) -- Bruce Ribner, director of infectious diseases at Emory University Hospital in Atlanta, and physician Kent Brantly speak at a news conference following Brantly's release from the facility where he was treated for the deadly Ebola virus. Brantly and aid worker Nancy Writebol had been evacuated from Liberia to Atlanta for treatment and are expected to make a full recovery. Writebol was released on Aug. 19, Ribner said. (Video courtesy of APTN. Source: Bloomberg)[/caption]
Aug. 21 (Bloomberg) -- Bruce Ribner, director of infectious diseases at Emory University Hospital in Atlanta, and physician Kent Brantly speak at a news conference following Brantly's release from the facility where he was treated for the deadly Ebola virus. Brantly and aid worker Nancy Writebol had been evacuated from Liberia to Atlanta for treatment and are expected to make a full recovery. Writebol was released on Aug. 19, Ribner said. (Video courtesy of APTN. Source: Bloomberg)[/caption]Ebola has a specific smell, says Sebastian Stein, a medical worker in Sierra Leone. While he can�t really describe it, he can tell you the effect.
�It�s full on. It�s in your face,� he said.
Sulaiman Kanneh Saidu, who runs an Ebola treatment center, recalls running to a police station to escape an angry mob when he tried to move a diagnosed patient, along with other suspected cases, to a hospital. The mob wanted the patients treated at home, and that�s where they ended up, he said.
At the front lines of the Ebola outbreak, doctors and support workers across Sierra Leone, Liberia and Guinea face a daunting challenge. On a daily basis, they deal with patients who lie about their travel history, hopeful their fever has nothing to do with the funerals they attended. They face suspicion from families who mistrust them and neighbors who fear them. And they are frustrated by a lack of adequate supplies and the tough conditions they work under.
In Liberia, some centers are running short of body bags, according to the government. In Sierra Leone, where Stein and Saidu work, patients are housed in clusters of tents, treated by medical staff who work tightly wrapped in head-to-toe plastic suits in 80-degree temperatures.

Medicins Sans Frontieres medical staff members wear protective clothing at the MSF...Read More
Early in the outbreak, �it was very depressing to be inside the wards because almost everyone died and there was blood everywhere,� said Stein, 33, who works with�Doctors Without Borders�after arriving in West Africa in June.
Numbers Cured
Now, the workers are more upbeat, according to Stein. They try not to count the dead, he said, �we are instead talking about the number of cured.�
While�1,350 people�had died from Ebola in West Africa as of Aug. 18, the fatality rate is shrinking as more and more people seek medical care earlier. As of last week, the�World Health Organization�reported�that about 47 percent recover with the help of early supportive treatment, a change from the mere 10 percent who survived in earlier outbreaks.
There are two Ebola centers in Sierra Leone, which has seen 907 cases, ranking it second among the three affected countries, and 374 deaths. One in Kailahun, on the eastern border, is run by Doctors Without Borders and a second, run by the government in Kenema, a major city.
Stein�s main job at the Kailahun site is overseeing sanitation protocols, including the removal of the dead. While conditions have improved over the last month, they remain challenging, he said by telephone.
 Source: MSF via Bloomberg
Source: MSF via BloombergThe disease �has a specific smell,� said Stein, who works with the aid group Doctors...�Read More
Five doctors, supported by nurses, treated more than 300 patients there in the last two months, about 200 of which were confirmed with Ebola.
80 Beds
For the most part, their work is done in tents that hold about 80 beds, with patients separated by canvas walls. The medical workers, who must wear head-to-toe plastic suits, masks, gloves and boots for most of the day in 80-degree temperatures, begin each morning at 6 a.m., Stein said, and the last shift ends at 10 p.m.
The bulk of the work force at Kailahun is Stein�s team of about 100 hygienists who spend their days cleaning up vomit and diarrhea, disinfecting beds and handling dead bodies. Many in the group are in their early 20s and have no prior training.
With borders closed and companies scaling back work schedules, Ebola centers are sometimes the only place to find work, according to Stein. The jobs pays as little as 37,000 leones a day, or about $8.50.
�Maybe they�ve never had a job before, and suddenly they�re confronted with a lot of death and suffering,� he said of his young team.
Ebola Reality
In many cases, medical workers say, the initial barrier they came up against was getting people to believe that Ebola was real. This is the first�outbreak�in West Africa and Ebola�s initial symptoms -� fever, headaches, diarrhea -� could belong to a wide range of diseases endemic to the region.
�People say, �Well, we�ve had fever, and we�ve always dealt with it this way, why should this be different?�� said Meredith Dyson, health program manager for Catholic Relief Services in Sierra Leone. �Once isolation units popped up, that created a lot of anxiety because they couldn�t access their loved ones.�
Typically in Sierra Leone, relatives bring food and fresh clothing to sick family members, so the total isolation required was also a source of distrust, Dyson said.
The lack of information about the disease was so widespread that when the first patient was announced to have the disease in Sierra Leone, the people of Koindu, a trading hub close to the border, attacked the health workers who were trying keep the infected patient isolated, including Saidu, the supervisor of the Ebola Management Center there.
First Case
Saidu had eight patients in his center in May, all suspected to have the deadly virus that had first appeared in neighboring�Guinea. When blood tests returned showing one, a woman, was the first in the country to be infected with Ebola, Saidu decided to take all of the patients to the treatment center in the city of Kenema, four hours away.
�The community interpreted it differently,� believing that anyone with Ebola would definitely die, he recalled. �They attacked us. We escaped and then went to seek refuge in the police station.�
In the end, he said, the patients were taken to their neighborhoods to be cared for by relatives, he said.
Fleeing patients continues to be a challenge for medical workers, as contact tracing is a key method for containing the outbreak spread, said Michael Stulman, of Catholic Relief Services. The incubation period for the virus is 2 to 21 days, which means an infected person potentially could go for weeks before presenting end-stage symptoms.
The families �are bringing them home before they�re recovered,� Stulman said in an e-mail.
Educating Communities
Dyson, of Catholic Relief Services, trains local officials, church leaders, and community health workers to spread the word about Ebola prevention and also to help keep tabs on anyone who has come into contact with the infected.
In Newton, a small rural town, the Ministry of Health and Sanitation has set up a crude three-bed isolation unit made of blue canvas draped over wood scaffolding. Spaced around the tenting are large posters that exhort the locals in bold fonts.
�Together we can prevent EBOLA,� one says. �People with Ebola who go to the health facility EARLY have a better chance of survival.�
The weather in Sierra Leone is another challenge.
It is the rainy season now, and the constant downpour can clog masks and get into goggles, so staff members are forced to stay indoors or within roofed areas. At the same time, the temperature during the day hovers in the 80s.
�Body Decomposes�
�In the heat in Sierra Leone, the body decomposes very, very fast,� Stein said. Because the bodies remain extremely infectious, his team has to work quickly to wash the body in a strong chlorine solution, burn their personal items, then wrap the deceased in not one, but two body bags.
While Doctors Without Borders is relatively well equipped to handle such tasks, other towns and cities are not as prepared. In some of the hardest hit areas in Liberia, for instance, the government has noted a shortage of body bags.
The northern county of Lofa, which borders Guinea and Sierra Leone, has �absolutely no body bags,� Liberia�s Ministry of Health and Social Welfare said in an Aug. 17 report.
Fiona Mclysaght, country director for�Concern Worldwide�in Sierra Leone, has been working to stock up local clinics, which are often the first places people go when they are ill. Her Dublin-based relief group is providing basic supplies including masks and disinfectant to more than 100 provincial health clinics, she said in a telephone interview.
Little Protection
�In some cases they don�t even have gloves,� she said, a factor contributing to health workers falling ill.
Despite the bleakness of the situation, the aid workers say they are happy to celebrate each incremental success. To help family members stay connected with the infected, some health workers have brought patients mobile phones, or constructed transparent barriers or windows that relatives can look through, according to Dyson.
�That�s gone a long way� to helping improve community trust, she said.
Saidu, the worker who once hid in the police station to escaped a community mob, later contracted the disease and survived. He now tells people his story to help them realize that one can get Ebola and survive, especially with early care.
In the tent hospital run by Doctors Without Borders, Stein says the mood is beginning to lift. Patients are coming in earlier, he said, which helps their chances of survival. Out of the 200 Ebola patients they�ve treated, he says, about 30 percent have survived.
It�s a small number, smaller than the outbreak�s total survival rate, but the workers �savor the moments,� Stein said. �We try to dance with the patients, we try to make them laugh, and we celebrate every time someone is cured.�
By Bloomberg
The Iran Project is not responsible for the content of quoted articles.